Latest Research Reveals Breakthrough Treatments for Small Intestinal Bacterial Overgrowth
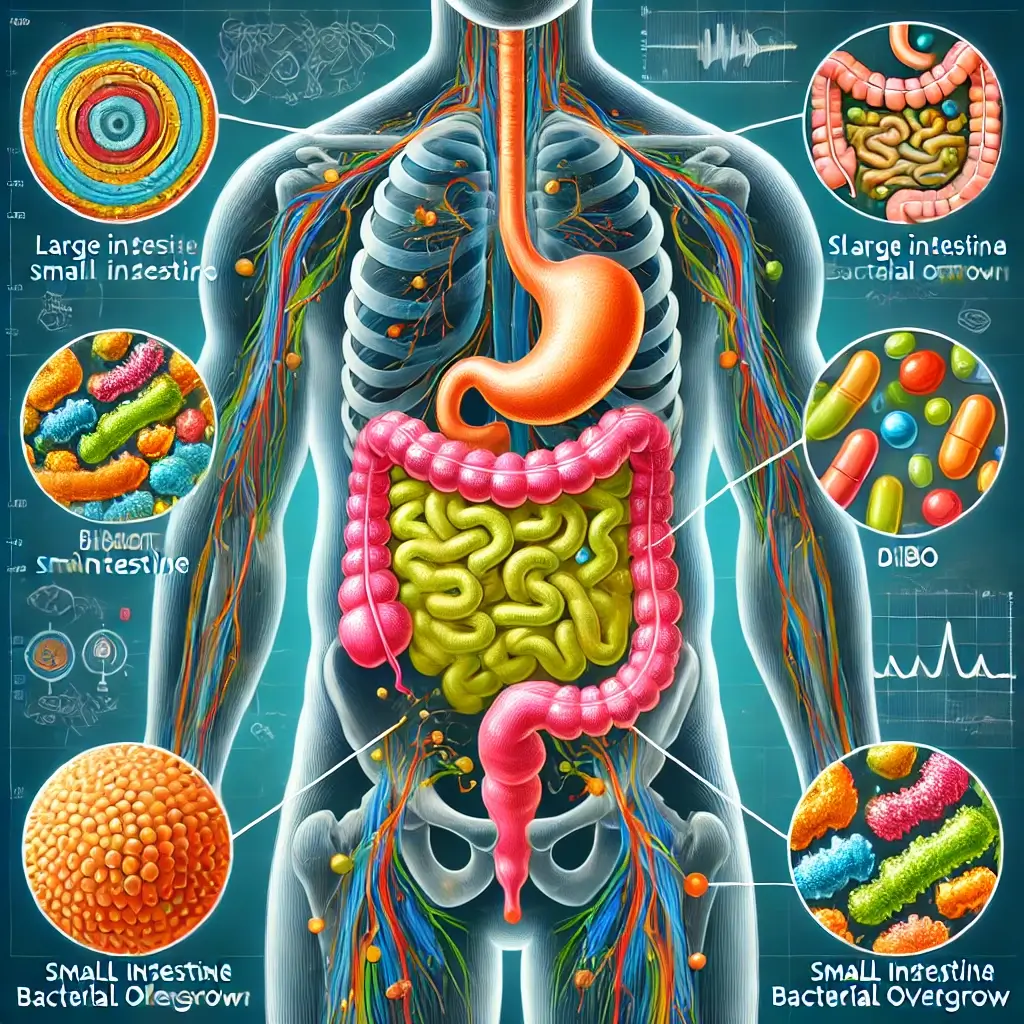
Understanding the Human Digestive System and SIBO
The human digestive system is a remarkable network where nutrients are absorbed, waste is eliminated, and a vast microbiome thrives. This ecosystem is finely tuned, with bacteria typically residing in specific sections of the gut. However, when this balance is disrupted, conditions like Small Intestinal Bacterial Overgrowth (SIBO) can arise. SIBO occurs when bacteria migrate from the large intestine to the small intestine or overpopulate the small intestine. This overgrowth interferes with digestion, nutrient absorption, and overall gut health, often leading to symptoms such as bloating, abdominal pain, diarrhea, and fatigue.
The Complex Nature of SIBO Management
The complexity of SIBO extends beyond its symptoms. It is a condition deeply influenced by factors such as motility disorders, dietary habits, and underlying medical conditions. Furthermore, its management requires a personalized approach that addresses not only the symptoms but also the root causes. This article delves into the multifaceted nature of SIBO, examines current research, and highlights effective treatment strategies to restore gut health and improve quality of life.
Research Findings on Causes and Risk Factors
Understanding the underlying causes of SIBO is essential for effective management. Impaired gut motility, often seen in conditions like gastroparesis and diabetes, is a major contributing factor. A study in Gut (2020) found that slow transit time increases the risk of bacterial colonization in the small intestine. Similarly, structural abnormalities such as intestinal adhesions or diverticula create environments conducive to bacterial overgrowth. Low stomach acid, another significant risk factor, is commonly associated with aging or chronic use of proton pump inhibitors (PPIs). Research published in The American Journal of Gastroenterology (2021) linked long-term PPI use with a higher incidence of SIBO, underscoring the importance of cautious medication use.
Diagnostic Challenges and Symptom Recognition
SIBO symptoms can mimic other gastrointestinal disorders, complicating diagnosis. Patients often report bloating, flatulence, abdominal discomfort, and irregular bowel movements, which are also common in conditions like Irritable Bowel Syndrome (IBS). A 2022 meta-analysis in Clinical Gastroenterology and Hepatology highlighted the overlap between SIBO and IBS, estimating that nearly 40% of IBS cases may involve underlying SIBO. Breath testing for hydrogen and methane gases, which measures gases produced by bacteria in response to ingesting certain sugars, remains the standard diagnostic tool. However, it is not without limitations. Emerging technologies, such as analyzing volatile organic compounds in breath samples, show promise for more accurate and non-invasive diagnostics.
Effective Treatment Approaches
Treatment for SIBO involves reducing bacterial overgrowth, alleviating symptoms, and addressing underlying conditions. Antibiotics such as Rifaximin are highly effective for hydrogen-dominant SIBO, with studies showing symptom relief in up to 70% of cases (Rezaie et al., 2017). For methane-dominant SIBO, a combination of Rifaximin and Neomycin is often used. Dietary interventions, particularly the low-FODMAP diet, play a crucial role in managing SIBO symptoms. This diet limits fermentable carbohydrates that bacteria feed on, reducing bloating and gas. A 2021 study in Nutrients emphasized the importance of professional guidance when implementing this diet to avoid nutritional imbalances. Probiotics are increasingly explored as a complementary treatment. A 2023 study in Alimentary Pharmacology & Therapeutics reported that certain strains, such as Bifidobacterium longum and Saccharomyces boulardii, may support gut motility and reduce inflammation, offering a potential benefit for SIBO management.
Strategies for Long-Term Management
Preventing SIBO recurrence requires addressing its root causes. Treating conditions like diabetes, hypothyroidism, or intestinal adhesions is vital. Lifestyle modifications for gut health, including stress management, regular physical activity, and adequate sleep, are equally important for maintaining gut health. A balanced diet rich in diverse plant-based foods can also help sustain a healthy microbiome.
Future Directions and Patient Care
SIBO is a multifaceted condition that demands a nuanced approach to diagnosis and treatment. Advances in medical research are shedding light on its complex mechanisms, paving the way for more targeted and effective therapies. From antibiotics and dietary modifications to probiotics and lifestyle changes, a comprehensive treatment plan tailored to the individual is essential for managing SIBO and preventing recurrence. As awareness of SIBO grows, so does the potential for earlier diagnosis and better outcomes. Patients are encouraged to maintain open communication with healthcare providers and to stay informed about the latest advancements in research and treatment. With a holistic and personalized strategy, SIBO can be effectively managed, restoring digestive balance and enhancing overall well-being.
Research Citations
References:
Rezaie, A., et al. (2017). Hydrogen and methane-based breath testing in gastrointestinal disorders: The North American consensus. The American Journal of Gastroenterology, 112(5), 775–784. https://doi.org/10.1038/ajg.2017.46
Gut. (2020). Impaired motility and bacterial overgrowth in the small intestine. https://gut.bmj.com/
Clinical Gastroenterology and Hepatology. (2022). Overlap of SIBO and IBS in gastrointestinal disorders. https://www.cghjournal.org/
Nutrients. (2021). Low-FODMAP diet in SIBO management: Benefits and challenges. https://www.mdpi.com/
Alimentary Pharmacology & Therapeutics. (2023). Probiotic interventions in SIBO treatment. https://onlinelibrary.wiley.com/
The American Journal of Gastroenterology. (2021). Proton pump inhibitors and SIBO risk. https://journals.lww.com/ajg